Understanding Bipolar 1 Disorder According to the DSM-5
Introduction
Bipolar 1 Disorder, classified as a mood disorder by the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition), is a complex and challenging condition. In this professional guide, I will provide an in-depth understanding of Bipolar 1 Disorder, including its diagnostic features, risk factors, symptoms, and treatment options.
Diagnostic Features
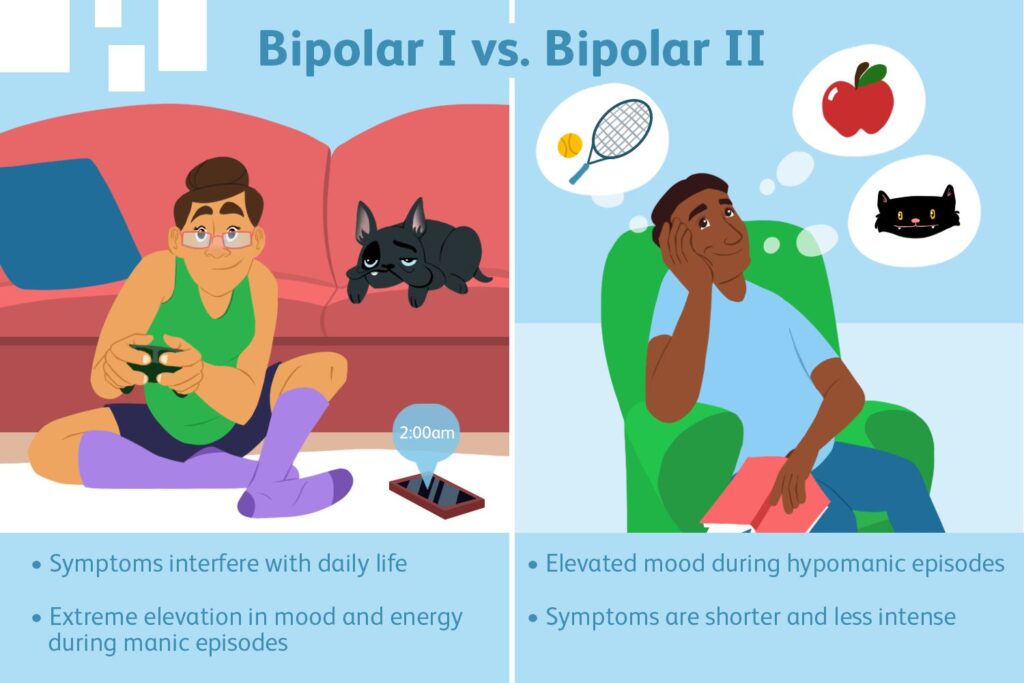
Diagnostic features for this condition include manic episodes, depressive episodes, and hypomanic mood episodes.
1. Manic Episodes
Firstly, for an individual to be diagnosed with Bipolar 1, they should exhibit a distinct period of abnormally elevated, irritable, and expansive mood lasting for at least one week and present nearly daily. During these periods, these individuals display enhanced impulsivity and energy as well as a decreased need for sleep. Examples of increased energy in this period include;
During manic episodes, an individual with Bipolar 1 may also exhibit a mood disturbance that causes impairment in social and occupational interactions. This kind of disturbance sometimes requires hospitalization to prevent self-harm or suicide. Lastly, for an individual to be diagnosed with Bipolar 1, their condition should also not be attributed to various physiological impacts of substances and drugs.
2. Major Depressive Episodes
For an individual to be diagnosed with Bipolar 1, major depressive episodes are also examined. According to the DSM-5, for one to be diagnosed with Bipolar 1, five of the below symptoms should be exhibited in the same 2nd week period. At least one of the symptoms should be a depressive mood or a loss of pleasure and interest. they include;
The above symptoms should also have the ability to cause clinically significant distress or impairments in occupational and social functioning. Lastly, the major depressive episode should not be linked to any physiological effects of substances or other medical conditions.
Hypomanic Episode
The hypomanic episode is similar to the mania one. However, an individual’s daily functioning is not impacted in this episode. During this episode, an individual with Bipolar 1 experiences abnormality in terms of irritable mood, increased energy, and activeness that lasts for about four consecutive days, occurring every day.
Three of the symptoms below should persist during this period of hypomanic episodes. They include;
- Inflated self-esteem or grandiosity
- Excessive involvement in activities that may result in adverse consequences
- Talkativeness
- High distractibility
- Decreased need for sleep
- Increased goal-oriented activities and
- Flight of ideas
This episode is also marked with an abrupt change in functioning that seems abnormal to them, mood disturbance, not severe enough to cause marked impairment in social and occupational functioning, and the episode should also not be attributed to physiological impacts of substances and drugs.
Risk Factors
Understanding Bipolar 1 risk factors can assist in the identification of people at higher risk and guide preventative measures. While the main cause of Bipolar 1 disorder remains elusive, several factors contribute to its development:
1. Genetic Predisposition
As per past research, there is a correlation between genetics and the development of Bipolar 1. According to the DSM-5, A family history of Bipolar 1 remains the strongest and most consistent risk factor for the condition’s development. There is a 10-fold increased risk of the condition among people with relatives with Bipolar 1 or 2. Unfortunately, the magnitude of Bipolar 1 risk increases with the degree of kinship. Even though having a family member with Bipolar 1 is a risk factor, having this genetic predisposition does not guarantee that one will develop the disorder.
2. Neurochemical Imbalances
Past studies have also argued that neurotransmitter imbalances, including dopamine and serotonin, play a role in Bipolar 1 Disorder. These imbalances can affect mood regulation, resulting in manic and depressive episodes.
3. Environmental Triggers
Environmental factors, including income, are also key factors. In addition, stressful life events, trauma, and substance abuse are also known to trigger the onset or exacerbation of Bipolar 1 Disorder, especially among susceptible individuals. According to the DSM-5, high-income individuals, separated and divorced, are also at a higher risk of developing Bipolar 1 than the general population.
Bipolar 1 Treatment Options
The treatment of this disorder mainly aims at stabilizing the patient’s mood and reducing the severity of the experienced symptoms. In this case, the treatment goal is to assist patients to function effectively in their day-to-day activities.
Bipolar 1 Disorder management involves a combination of therapeutic approaches tailored to the patient’s individual needs. These therapeutic options include medications, psychotherapy, lifestyle modifications, and, in rare cases, Electroconvulsive Therapy.
Medication
Over the years, various medications have been used to not only manage Bipolar 1 symptoms but also to stabilize the patient’s mood. Medications such as mood stabilizers lithium, antidepressants, 2nd generation antipsychotics, and anticonvulsants to relieve mania may be prescribed for a patient depending on their disease progression and phase.
Psychotherapy and Counseling
Psychotherapy and counseling have also been used to equip people with bipolar 1 to manage the condition effectively. One of the most effective approaches for Bipolar 1 is the Cognitive-behavioral Therapy (CBT). Using CBT, therapists teach patients to;
- Identify and change negative thoughts
- Improve self-awareness
- Mood stabilization
- Effective problem solving among others
Another approach linked to CBT is psychoeducation, which offers knowledge and coping strategies to patients. Psychoeducation helps patients in;
- Understanding their condition, its nature, potential causes, and impacts on behaviors and emotions
- Symptom recognition – early disease recognition and treatment results in better outcomes and prevents severe episodes.
- Medication management – Psychoeducation helps patients know medication’s role in Bipolar 1 treatment, drug side effects, and the adverse impacts of non-adherence.
- Coping skills, including emotion regulation, stress management, and effectively handling triggers
- Relapse prevention
- Stigma reduction
- Enhanced quality of life.
- Lifestyle Modifications
Another approach to managing Bipolar 1 is lifestyle modification. Such includes regular sleep patterns, stress management techniques, and avoiding alcohol and substance abuse. In addition, a supportive social network is also crucial when dealing with this condition.

Electroconvulsive Therapy (ECT)
ECT is one of the rarest approaches to managing Bipolar 1. This approach is mostly undertaken when other treatment approaches are ineffective. This procedure involves passing electrical currents through the brain to induce controlled seizures, which works towards alleviating Bipolar 1 related symptoms.

Conclusion
Understanding Bipolar 1 Disorder, according to the DSM-5, is a critical step toward the condition’s effective diagnosis and treatment. As indicated above, Bipolar 1 is a complex mood disorder characterized by alternating manic and depressive episodes. The disorder has a few risk factors, including genetic, neurochemical, and environmental factors. Knowing the condition’s symptoms and risk factors can help individuals seek timely intervention and improve their quality of life.
If you or someone you know is experiencing symptoms of Bipolar 1 Disorder, consulting with a qualified mental health professional is essential. With proper treatment, support, and self-care, people living with Bipolar 1 Disorder can effectively manage their condition and lead fulfilling lives.